Dr. Heidi Larson, director of the Vaccine Confidence Project, described data from a recent Pew Center study, instructing us to “HANDLE WITH CARE!” as if a jeweled Fabergé egg and not a series of sampled statistics.
The study’s title: “Americans’ Trust in Scientists, Other Groups Declines.”
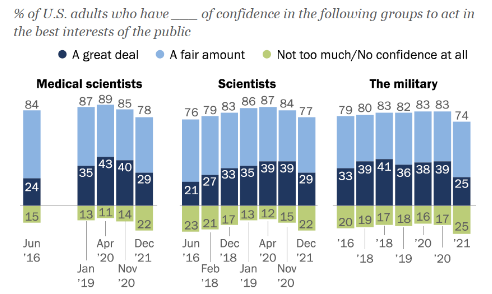
Credit to: Brian Kennedy, Alec Tyson, and Cary Funk
“Once seemingly buoyed by their central role in addressing the coronavirus outbreak,” Pew Center researchers write, the public’s trust in scientists and health professionals has sunk. This phenomenon is not confined to remote corners of Twitter or the turbulent backwaters of a few Facebook community chats. No, it’s palpable in the media, in conversation, in our collective consciousness. Why is this? And why now?
Last month, The Duke Global Health Institute hosted a few health experts to answer these questions in the “Building Trust in Public Health: A Post-COVID Roadmap” panel. Jack Leslie, a visiting fellow at the Duke-Margolis Center for Health Policy, contextualized declines in public trust, citing increased populism and anti-elitism. It’s not difficult to chart the evolution of this zeitgeist. In the past three decades alone, Americans have become completely cocooned in media.

CNN’s Ted Turner (i.e. the ‘Mouth of the South’) is accredited with the genesis of the 24 hour news cycle. He notably “didn’t bargain for… [the] insomniacs,” writes journalist Lisa Napoli, nor did he bargain for its longevity, or our inability to escape it. From coverage of the Iraq War to the OJ Simpson investigation to political partisanship in Washington, and of course, to COVID-19.
The erosion of institutional faith is not unique to the government but, like an acid rain, weathers indiscriminately. It eats away at trust in churches, corporations, media institutes, universities, K-12 schools, etc. In fact last semester, I attended another Duke panel entitled “Policing the Pages,” in which increased polarization across the US contributed to concerted efforts to bar certain books (often those with LGBT and minority characters) from elementary school libraries and syllabi. A kind of censorship akin to dress codes and mandatory veggies in bagged lunches.
This sentiment, unlike COVID-19, is not novel. Leslie described a “trifecta” of events, slowly chipping away at public trust: 1) the great recession of ‘08, 2) waves of immigration in the United States and Europe, and finally, 3) the pandemic.
For decades, and with little exception, science was lauded as infallible, an authority, bridging turbulent seas of dis- and mis-information. It was well-mannered, professorial, clad in wire-rimmed glasses and bowtie. “We had pretty high trust in scientists and public health institutions prior to the pandemic… relative to other institutions which have taken a hit over the past twenty years,” Leslie acknowledged.
Of course, this no longer is the case.

Dr. Heidi Larson collected this pathos in anecdotes for the Global Listening Project, an oral history of personal pandemic experiences. Many described “…a feeling of disconnect with the government. [They] would give us these directives, but people felt they had no connection with their reality, their situation.” Larson, for example, recognized patterns of isolation in schools. There was a pervasive sense that neither legislator nor scientist had stepped foot into these schools before creating policies. Bureaucratic deflection so to speak.
Larson consequently felt a shift in COVID-19 rhetoric. What once was “upholding global unity,” “encouraging communal cooperation,” and “assuring responsive governance” became, as Larson put it, “getting a jab in the arm.” The disconnect between the Joe Publics, the John Qs, and their public institutions began to feel especially cavernous as the pandemic stretched weeks, months, then years.
This begs the question, how can we rebuild trust in public health?

Dr. Rispah Walumbe, a global health policy and advocacy specialist, described the “orchestration” of multisectoral partnerships during the pandemic (in Africa, specifically) that combined “state and non-state actors with public and private sector actors and, of course, those on the social, economic, and political sides.”
She found that, at the start of the pandemic, trust was enhanced. The virus was identified as a “key problem” and was, to some degree, universally threatening. A conduit of centralized communication followed. As the pandemic elongated, the discrepancy between the populations disproportionately burdened by COVID (poor and minority communities) and those not so much grew wider. Communication became less effective. Still, Walumbe advocated for the continuity of engagement between health institutions and the public in the aftermath of the pandemic. Peel back the Oz-like bureaucratic curtains and increase transparency.

Dr. Mandy Cohen, Secretary of North Carolina’s Department of Health and Human Services, agreed. In recent studies, she explained, NC ranked 2nd among the states for its general safety during the pandemic, which she attributed to the state’s prioritization of public trust. “Before we even had our first case, we were talking about how our crisis response was going to hinge on whether we could build and maintain trust with the public… we tried to be really tactical about trust, which can feel ephemeral and fleeting… and really broke it down into three buckets. The first was transparency, the second was competency, and the third was relationships.”
Rebuilding trust in public health, thus, seems less a roadmap and more a spigot. Institutions must continue to fill the buckets Cohen described.
As the pandemic ebbs, however, the ubiquity of isolation, anxiety, and turmoil cannot be understated. A recent WHO article characterized this pervasive fear as “contagious,” pathologic, a kind of virus itself.
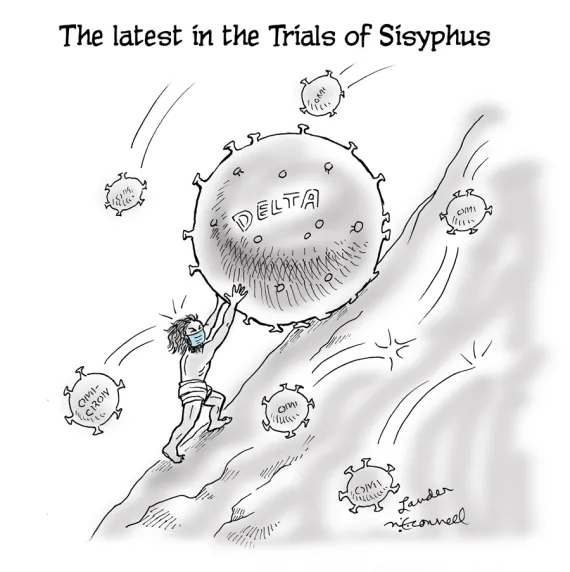
In an age of mass misinformation, public health officials, doctors, and scientists now stand with the Sisyphean task of restoring public trust. And the panelists concurred: it is fragile. Volatile even.
Yet, as illustrated in this article, it is not elusive. Prioritize communication. Prioritize transparency. Prioritize competency, relationships, and community engagement.
I will defer to Walumbe who put it best during the conversation: “These institutions do not operate in a vacuum. Community is pivotal in thinking through trust, it’s how we’re organized across the world… that’s something that is critical in how we approached COVID-19 challenges…” and, presumably, in how we should continue.
Thank you to the panelists, moderator Dr. Krishna Udayakumar, and Dr. Mark McClellan, Director and Robert J. Margolis, M.D., Professor of Business, Medicine and Policy at the Margolis Center for Health Policy.

Post by Alex Clifford, Class of 2024
